Connie: Good evening, dear friends. Thank you for tuning in to our show. Today, we invited Professor Hofstadter to our program. Thanks for joining us, Dr. Hofstadter.
Dr. Hofstadter: Thanks for having me. Hello, everyone. I’m very excited to be here.
Connie: The definition of probiotics was evolved during the last few years. The food and agriculture organization and world health organization well-defined probiotics as the “creation of a product comprising feasible, specified microorganisms in adequate quantities that modify the microflora in the host section and thus have helpful health effects in the host”. Recently, probiotics have been re-defined as “Live bacterial strains with healthiness effect on the host when they ingest sufficient amounts daily and are combined into gut microbiome”. The foremost genera of probiotics are Lactobacillus and Bifidobacterium and several fitness assistances have been investigated using in vitro models or different in vivo models, for example, modulation of the immune system, lessening of cholesterol, antioxidant, and also anti-carcinogenic activity levels. Today, we are going to discuss gut microbe and probiotics as bio-therapeutics for non-alcoholic fatty liver disease. And before we start today’s discussion, can you give us an overview of what a non-alcoholic fatty liver disease is?
Dr. Hofstadter: Sure. This is a serious problem. Non-alcoholic fatty liver caused by obesity has become a global health problem for both adolescents and adults. It refers to a kind of clinical-pathological syndrome characterized by excessive fat deposition in liver cells caused by alcohol and other clear liver damage factors. Non-alcoholic fatty liver disease can directly lead to decompensated liver cirrhosis, hepatocellular carcinoma, and recurrence of the transplanted liver, and it can also affect the progress of other chronic liver diseases and participate in the pathogenesis of type 2 diabetes and atherosclerosis.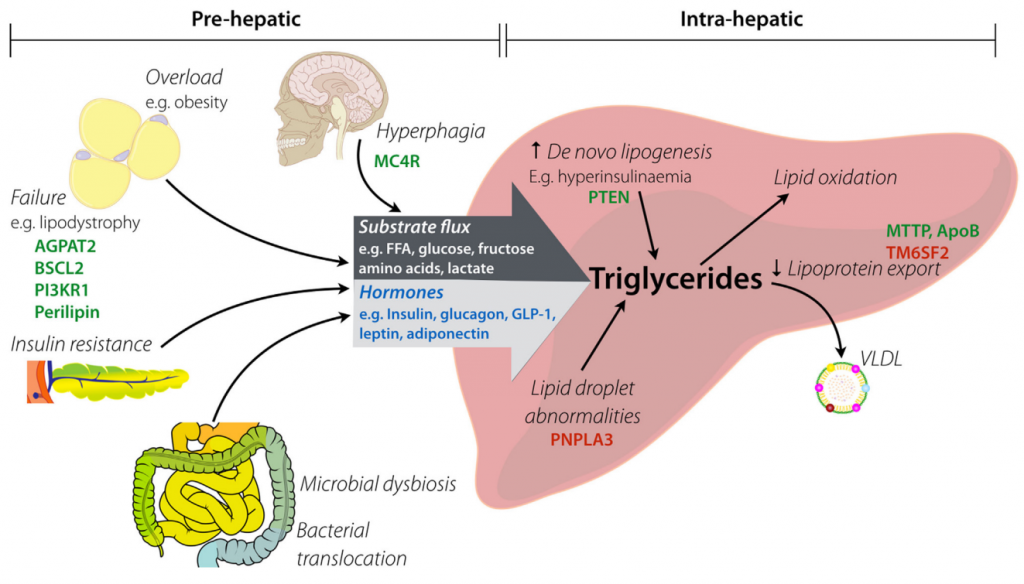
Connie: It does sound very serious. In addition to environmental and genetic factors, the gut microbe plays an important role in non-alcoholic fatty liver disease development and progress. Till now, there is no medical therapy approved for non-alcoholic fatty liver disease treatment and the primary therapeutics are exercise and dietary management. I’m actually a bit shocked at this.
Dr. Hofstadter: Well. What I am going to introduce might shock you even more. Non-alcoholic fatty liver is a multifactorial disease and its pathogenesis is still unclear. “Two-striker-like hypotheses” is one of the original hypotheses for non-alcoholic fatty liver pathogenesis because steatosis is the first strike and oxidative pressure is the second hit. However, in the intestine of human adults, the correlation between changes in gut microbiota and non-alcoholic fatty liver disease pathogenesis has been identified in a range of research.
Connie: Can you elaborate more on this?
Dr. Hofstadter: Yeah. Researchers just found out the phenomenon in non-alcoholic fatty liver disease patients, stages of fecal Bradyrhizobium, Propionibacterium acnes, Dorea, Peptoniphilus, Anaerococcus, Ruminococcus increased, and lower proportions of Rikenellaceae and Oscillospira increased as well. In another study, they found that patients with obesity and non-alcoholic steatohepatitis had different ratios of Firmicutes, Bacteroides, Actinobacteria, and alcohol-producing bacteria in comparison to the vigorous patients.
Connie: It suddenly occurred to me that we can see whether it will affect the non-alcoholic fatty liver disease from the metabolism of gut microbiota. Most of us should know that organic acids are the main metabolites of fructose and other fermentation sugars. This metabolic process is carried out by a large amount of gut microbiota accumulated in the intestine. These organic acids include lactic and succinic acids, fatty acids including ethanoate, propionic acid, and butyric acid, and ethanol. I suppose that these metabolic productions must play some roles. Do you think?
Dr. Hofstadter: Yes, of course, they do. Lactate, acetate plays a crucial function in the metabolic cross-feeding pathways of bacterial organisms such as Anaerostipes caccae, Eubacterium hallii, and the Roseburia sp. And you know another metabolic product, short-chain fatty acids, can attenuate the accretion of triglycerides in hepatic cells via increasing the ratio of propionate to acetate which could inhibit lipogenesis.
Connie: Then what about ethanol and acetaldehyde?
Dr. Hofstadter: They are essential sugar fermentation metabolites used by various gut microbiota, such as heterotactic intestinal bacteria. Ethanol can be absorbed into acetate and also acetaldehyde. Acetaldehyde may result in increased blood circulation leading to liver injury.
Connie: Do you mean that ethanol may have two sides in modulating disease occurrence?
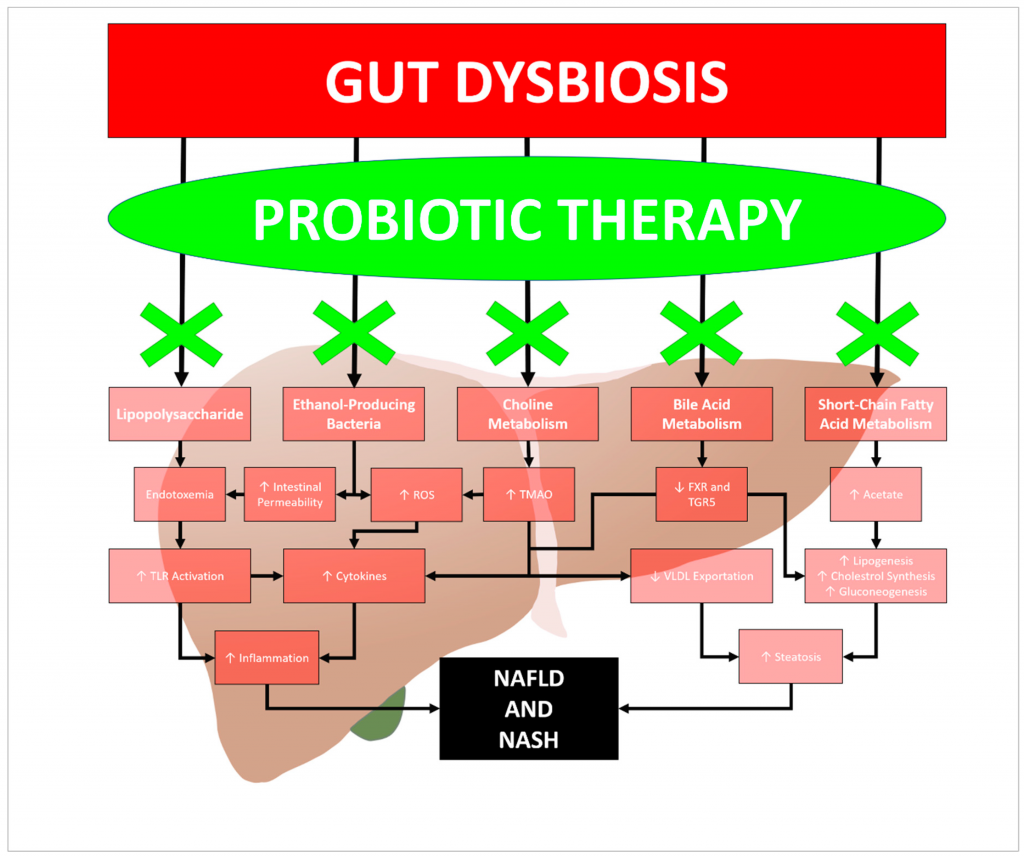
Dr. Hofstadter: Well, not really. You might be thinking about the opposite function of ethanol conversion products. In general, studies have agreed that ethanol can promote the occurrence and development of nonalcoholic fatty liver disease. There is research indicating that ethanol provided by intestinal microbiota in patients with non-alcoholic fatty liver disease had contributed to non-alcoholic fatty liver disease production. Another research also found that non-alcoholic steatohepatitis patients had improved alcohol-generating bacteria that increased serum levels of alcohol and increased oxidative stress. Interestingly, it was found that the non-mannitol generating intestinal hetero-fermentative lactobacilli were observed to generate large quantities of ethanol from the fermentation of fructose in obese fecal slurries.
Connie: Interesting. You mentioned earlier the concept of “second hit” in the “two-strike hypotheses”, which is oxidative pressure. What is the relation between gut microbiota and oxidative pressure?
Dr. Hofstadter: Well. Gut microbiota fermentation of dietary fructans may stimulate glucagon hormone such as peptide-1 and also peptide YY. They also enhance glucagon secretion such as peptide-2, which plays a vital part in enhancing the colonic integrity and tight junction as well as reducing blood circulation of lipopolysaccharide. Lipopolysaccharide is the active component of endotoxin. And lipopolysaccharide endotoxin produced by Gram-negative Intestinal bacteria could induce different pro-inflammatory cascades-associated non-alcoholic steatohepatitis.
Connie: I see. You suggest that probiotics can be used as a strategy to reduce the risk of non-alcoholic fatty liver disease. Has it been confirmed by any specific studies?
Dr. Hofstadter: Definitely. A range of animal models has been conducted to test the impact of various probiotic strains on non-alcoholic fatty liver disease risk reduction. Among them, researchers found Akkermansia muciniphila. They regarded it as one among the next generation probiotics, so you can imagine how amazing the effect it could have. Akkermansia muciniphila regulates different metabolism pathways of the host either in the living or pasteurized form, whereas both forms could reduce the body and fat mass gain as well as reduce serum triglycerides and abstaining glucose, also enhance insulin sensitivity in mice.
Connie: That really is amazing. Then what is changed by Akkermansia muciniphila from a molecular perspective?
Dr. Hofstadter: Akkermansia muciniphila could improve the gut barrier in 3 ways. They could enhance the countenance of constricted connection of protein together with occludin, claudins, and tight junction protein 1, tight junction protein 2, and tight junction protein 3. And they can reduce the circulation of endotoxemia such as lipopolysaccharide stages. Then finally, they can inhibit inflammatory reactions resulting in increased glucose and fat metabolism.
Connie: This is promising to some extent. But of course, we still need further work on the mechanism through which probiotics could reduce non-alcoholic fatty liver disease risk. So much for our content today. Thanks, Professor Hofstadter, for your time and great input. And thanks everyone for listening. We will continue our discussions next week. Until then!
