Connie: Dear friends, thank you so much for tuning into our program on this beautiful Saturday evening. Surely you all know our guest, Dr. Hofstadter. Thank you for joining us today, Dr. Hofstadter.
Dr. Hofstadter: Thank you for inviting me, Connie. Good evening, everyone. It is great to see you again. I’m very excited to be here.
Connie: So today and in a few of the coming episodes, we will discuss the positive effects of probiotics on some diseases or physiological conditions. In the last episode, Dr. Hofstadter introduced the beneficial effects of probiotics on patients with hypertension, urogenital tract infection, and lactose intolerance. Where should we start today?
Dr. Hofstadter: So what we will discuss today is closely related to the response of the immune system and gastrointestinal tract to prebiotics. How about we start from I give you a brief introduction to the relevant knowledge of the immune system. As we all know, the immune response in the host is caused by innate immunity after the entry of foreign particles such as pathogens or any tissue damage. However, an uneven immune response can lead to acute inflammation and unrestricted tissue damage and disorders.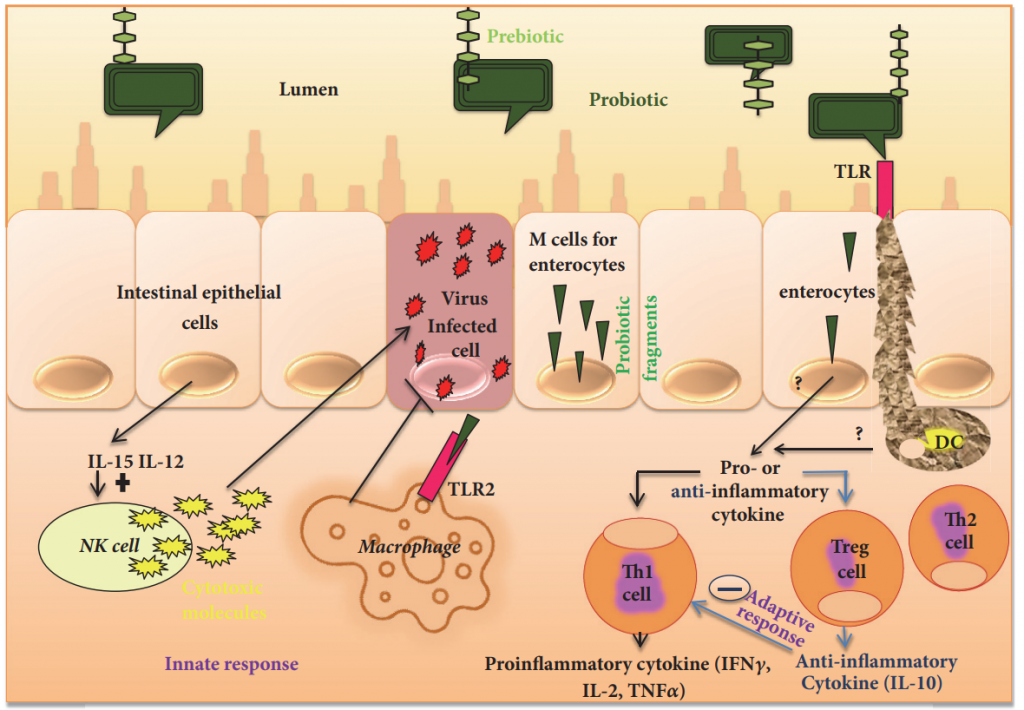
Connie: So, what role does the GI tract play in the immune system?
Dr. Hofstadter: In the GI tract, epithelial cells are the first barrier against pathogens. The mucosal immune system response is also carried out in the GI tract. Microorganisms can recognize microbe-related molecular patterns that exist on the surface of bacterial cells. They interact with the pattern recognition receptors of intestinal antigen-presenting cells such as macrophages and dendritic cells.
Connie: So we can say that most of the human immune system exists in the intestine. And a large number of immune cells such as T cells, B cells, and natural killer cells are concentrated in the intestinal mucosa. The intestinal tract is the first defense system of immunity. Remind us What is the mucosal immune system?
Dr. Hofstadter: In scientific terms, the mucosal immune system refers to the lymphatic tissues widely distributed in the respiratory tract, GI tract, genitourinary tract, and under the mucous membrane of some exocrine glands. It is the main place to perform the local specific immune function. The mucosal immune system is an important part of the body’s entire immune network. It is also an independent immune system with a unique structure and function. The mucosal surface is in direct contact with external antigens and is the body’s first line of defense against infection. Therefore, the mucosal immune system plays an extremely important role in fighting infections.
Connie: In other words, the mucosal immune system is the responsible sentinel?
Dr. Hofstadter: That’s right. It can distinguish between the harmless and harmful to decide whether to let it go or stop it.
Connie: How important is the mucosal immune system in the immune system?
Dr. Hofstadter: In terms of quantity, the mucosal immune system is the largest in the immune system, where the number of lymphocytes is more than the sum of other parts, and 60 percent of T cells work in the mucosa. So yes, it is pretty important.
Connie: What is the role of the mucosal immune system in the GI tract?
Dr. Hofstadter: The mucosal immune system’s perception of intestinal microbiota plays an important role in maintaining intestinal homeostasis and generating protective responses.
Connie: So, do you think probiotics help with the immune system of the GI tract?
Dr. Hofstadter: Simply put, probiotics can activate the mucosal immune response. I remember there was a study conducted in 2004 that showed that after attaching a potential probiotic strain to epithelial cells, the immune response is stimulated by the formation of toll-like receptors.
Connie: After probiotics adhere to the intestine, does it have any effect on the cytokine levels?
Dr. Hofstadter: Yes. After this adhesion, the production of cytokines such as interleukin-6 and macrophage chemoattractant protein-i is enhanced without changing the intestinal barrier.
Connie: In addition to toll-like receptors, what other ways can prebiotics stimulate the immune response?
Dr. Hofstadter: Prebiotics also stimulate dendritic cells and macrophages, which can lead to an increase in antibody immunoglobulin A. Cytokine secretion molecules from these bacteria also bind to receptors on dendritic cells to further activate different signaling pathways. Some probiotic strains, such as Lactobacillus rhamnosus, can induce heme oxygenase activity in dendritic cells. And next, you know, the mucosal T regulatory cells in the intestinal-associated lymphoid tissues are activated.
Connie: Probiotics were also reported to promote human health by producing low molecular weight compounds. Can you elaborate more on this?
Dr. Hofstadter: Sure. Probiotics can inhibit the growth of pathogenic bacteria through organic acids and antibacterial high molecular weight compounds, such as bacteriocins. For instance, according to reports, organic acids such as butyric acid, acetic acid, and lactic acid have strong anti-pathogenic activity by destroying gram bacteria such as Escherichia coli, Pseudomonas aeruginosa, and Helicobacter pylori. Some reported bacteriocins produced by probiotics are bifidobacteria B produced by bifidobacteria, nisin from Lactococcus lactis, lactomycin from Lactobacillus Plantarum and lactomycin B from Lactobacillus acidophilus.
Connie: I see. And we know that natural killer cells participate in both innate immunity and adaptive immunity. So, are natural killer cells also related to intestinal immunity?
Dr. Hofstadter: In fact, natural killer cells also interact with the gut microbiota. They affect the immune response mediated by adaptive T cells by acting on antigen-presenting cells. They are also affected by the lipid antigens present in the probiotic cells.
Connie: Does this mean that probiotics can enhance the activity of natural killer cells?
Dr. Hofstadter: Exactly. According to reports, lactic acid and heat-treated Lactobacillus plantarum can enhance the function of natural killer cells.
Connie: What is the mechanism by which probiotics have a beneficial effect on diseases, most commonly, you know, like allergies and colitis?
Dr. Hofstadter: I think this beneficial effect can be attributed to probiotics’ potential to enhance the production of T lymphocytes. For example, the probiotic strain B. longum improves colorectitis in animal models by adjusting the ratio of cytokines in T cells. Another example would be that, after healthy people consume Bifidobacterium infantis, the level of Foxp3 lymphocytes increases. This further leads to decreased levels of pro-inflammatory cytokines in patients with ulcerative colitis or psoriasis.
Connie: Is it true that prebiotics can regulate the response of T cells through their metabolites such as short-chain fatty acids?
Dr. Hofstadter: That’s right. In fact, short fatty acids such as butyrate can enhance the extrathymic production of regulatory T cells, and the de novo production of regulatory T cells is mimicked by propionic acid.
Connie: When it comes to probiotics, people often associate them with the digestive system and intestinal health, but now more and more studies begin to pay attention to their important role in the immune system. Studies have shown that probiotics can support immune function by promoting different aspects of the body’s natural immune defense. That’s it for our discussion today. Thanks, Dr. Hofstadter, for bringing us another great episode. And thanks everyone for listening. Please stay tuned for our next episode which will be happening at the same time next Saturday. See you then!
Dr. Hofstadter: Thanks everyone. I hope I will see you next time.
